Evidence-Based Nudges for Better Patient Outcomes

Overview
PATIENT ENGAGEMENT LANDSCAPE
The concepts of remote monitoring, telemedicine, and, as noted by The New England Journal of Medicine, automated hovering have been around for a while now. In the United States, health care funding promotes a reactive, visit-based model in which patients are seen when they become sick, usually during hospitalizations and outpatient visits. The care model fails not only because it is costly and often fails to prevent disease, but also because individual behaviors account for so much of health outcomes. Even patients with chronic illnesses may only spend a few hours a year with a doctor or nurse, but they spend 5,000 waking hours a year determining whether to take prescribed drugs or obey other medical advice, deciding what to eat and drink, whether to smoke, and other things that can have a huge effect on their health.
Meanwhile, clinicians are being asked to do more with less time. They often run behind schedule and suffer from decision fatigue. As noted by The Journal of the American Medical Association, a cumulative burden of making choices leads to worse decisions over time, and even the most knowledgeable and well-resourced doctors deliver care with gaps, such as overusing surveillance imaging in a cancer patient, failing to prescribe statins to a patient who meets the criteria, or prescribing an expensive medication when a less expensive alternative is accessible. Usually, these differences emerge not from a lack of judgement, experience, or poor intentions, but rather because doing it right all of the time is difficult, and practice environment design unwittingly makes guideline-concordant treatment harder — or at least not as easy as it should be. This is where nudges come into play.
Enabling personalized and measurable engagements through the Nudge Framework
True patient engagement should have observable performance metrics that can be measured over time. In general, this is still a concern. However, data being collected continues to demonstrate that patient engagement can be highly beneficial when performed in a coordinated manner. With the advent of devices to track activity, heart rate, and much more, the rise of AI to predict health issues from that flood of data, automation to “hover” over patients and so on, healthcare is on the cusp of putting patients where they belong — at the center of their own health (with some assistance).
It is possible to provide amazing care to any individual but it can come at a significant cost. Concierge care for all? Sure, but at what cost and who will pay that price? This is where advances in technology and “automated hovering” will play an increasingly important role. Programs such as Heart Safe Motherhood have been shown to reduce automated hovering costs significantly and reduce readmissions while not increasing clinician workloads.
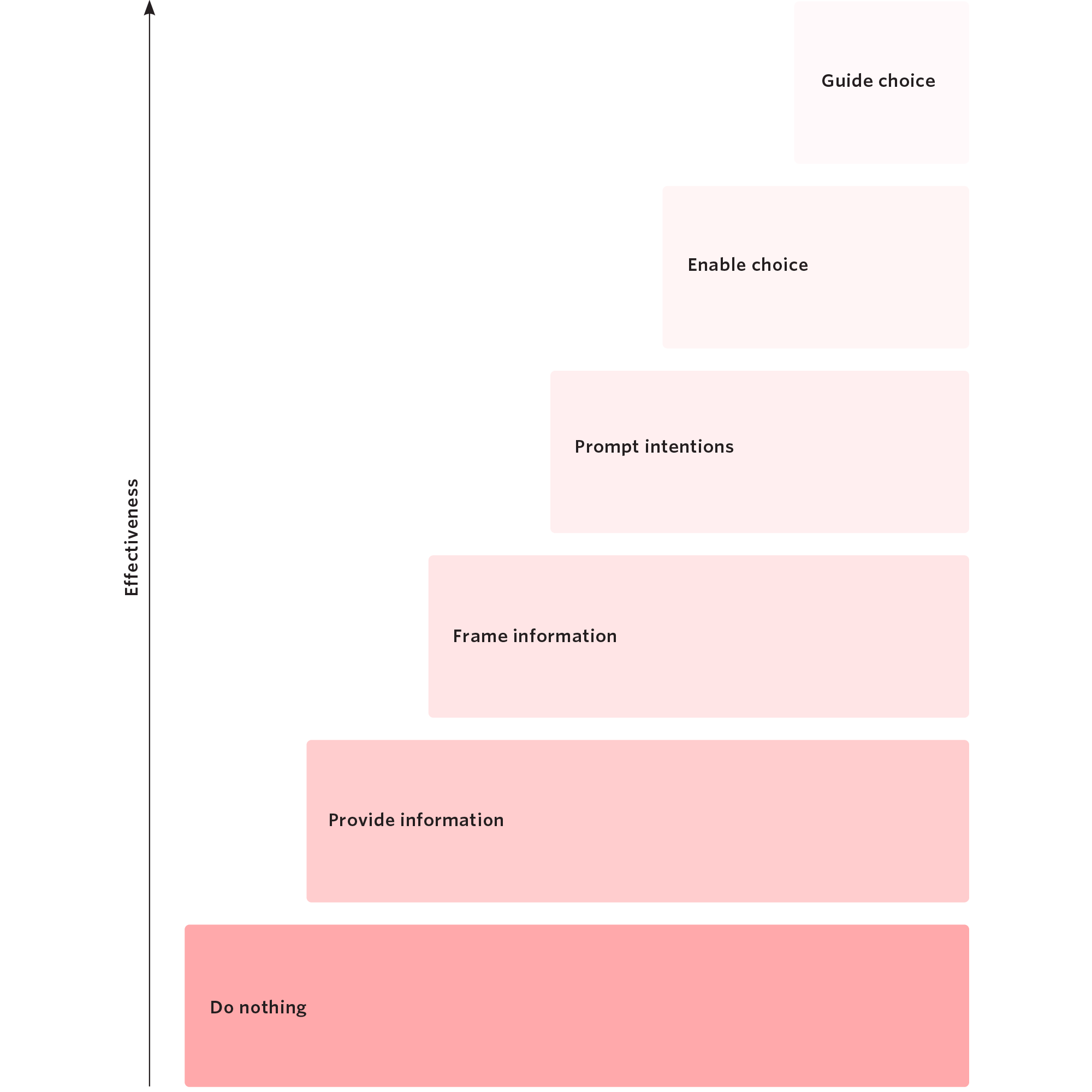
Guide choice through default options
Enable choice
Prompt implementation intention
Frame information
Provide Information
Do nothing
An example being to simply monitor cancer screening rates. This doesn’t provide much value except to establish a baseline. Most reports might fall into this category, i.e. there is rarely a “so what” question being answered by the report.
- In a randomized trial with overweight and obese adults from 40 US states, we used a behaviorally designed gamification intervention with competition to significantly increase physical activity during a 6-month period with sustained effects in the 3 months after the intervention stopped. Participants in the competition arm walked about 100 miles more than control during the study.
- In a randomized trial of elderly patients that recently had a heart attack or other ischemic event, we used loss-framed financial incentives and personalized goal-setting to increase physical activity during a 4-month intervention (1368 steps per day more than control) with sustained effects in the 2 month follow-up period (1154 steps per day more than control).
- In a randomized trial of adolescents and young adults with type 1 diabetes, we used loss-framed financial incentives to significantly increase glucometer adherence from 19% in control to 50% in the intervention group.
- In a randomized trial of primary care physicians, the trial used peer comparison feedback on clinician performance with automated patients lists to triple the prescribing of statin medications for patients that were at high-risk of cardiovascular events. This led to the health system wide adoption of these types of nudges for statin prescribing.
- In a randomized trial of radiation oncologists, the trial used nudges in the electronic health record to reduce the rate of unnecessary imaging in palliative cancer patients from 68% to 32%. This saved more than 3,000 unnecessary imaging tests per year.
- In a study of primary care practices, the study used nudges in the electronic health record to increase influenza vaccination rates by 9.5 percentage points. Across the entire health system, this led to 5000 more patients being vaccinated.
Ready to learn more?
Ready to learn more?
Please fill out the form to gain access to the complete Whitepaper